This article by Andy McDonnell was published in the Irish Independent on the 21st of June, 2024.
Unable to train collectively at the time, amid the Covid-19 pandemic, the Louth senior football panel, under new manager Mickey Harte, were instructed to do lone training sessions. They were tough and I remember coming to the end of the gruelling session in March 2021 in Newtown Blues’ pitch and feeling a pain in my right knee.
I didn’t hurt it by twisting or turning and it wasn’t an impact injury. I knew something was up and when I went home the pain intensified.
Initially, it was thought by the medical team that there was nothing wrong with my knee, but I knew something wasn’t right. I played through the pain barrier weeks later against Antrim in the first round of the National League. I didn’t perform great but played the whole game. I remember getting home afterwards and I was unable to move my leg. It took me 10 minutes to get from my car to the couch in the sitting room.
I suppose breaking my femur in 2009 and having a minor operation in 2017 for a meniscus tear on the same knee didn’t help my cause.
Numerous physio sessions, anti-inflammatory tablets, consultant appointments and steroid injections failed to work as the pain remained.
I was diagnosed with knee osteoarthritis, otherwise known as wear and tear. I had planned to finish up playing for good as it was affecting my day-to-day life.
I then met a Meath man in January 2022 who I owe a great deal to. Liam Hogan, a physiotherapist, looked at my knee and to me I’d be back playing within six or seven months. I laughed at his optimism but told him I’d do everything I could.
A few weeks in and I wasn’t completing the rehab as planned. Liam was quick to call me out and told me not to be wasting his time. As the saying goes, “you only get out of it what you put into it”.
After consistently doing my rehab, my mindset changed as I started to feel the benefits of it. Eventually, I could walk pain free. My progress continued steadily and I made my comeback in a league match against Mattock Rangers in June 2022. Liam was in attendance and it was great to be back after a torturous 14 months.
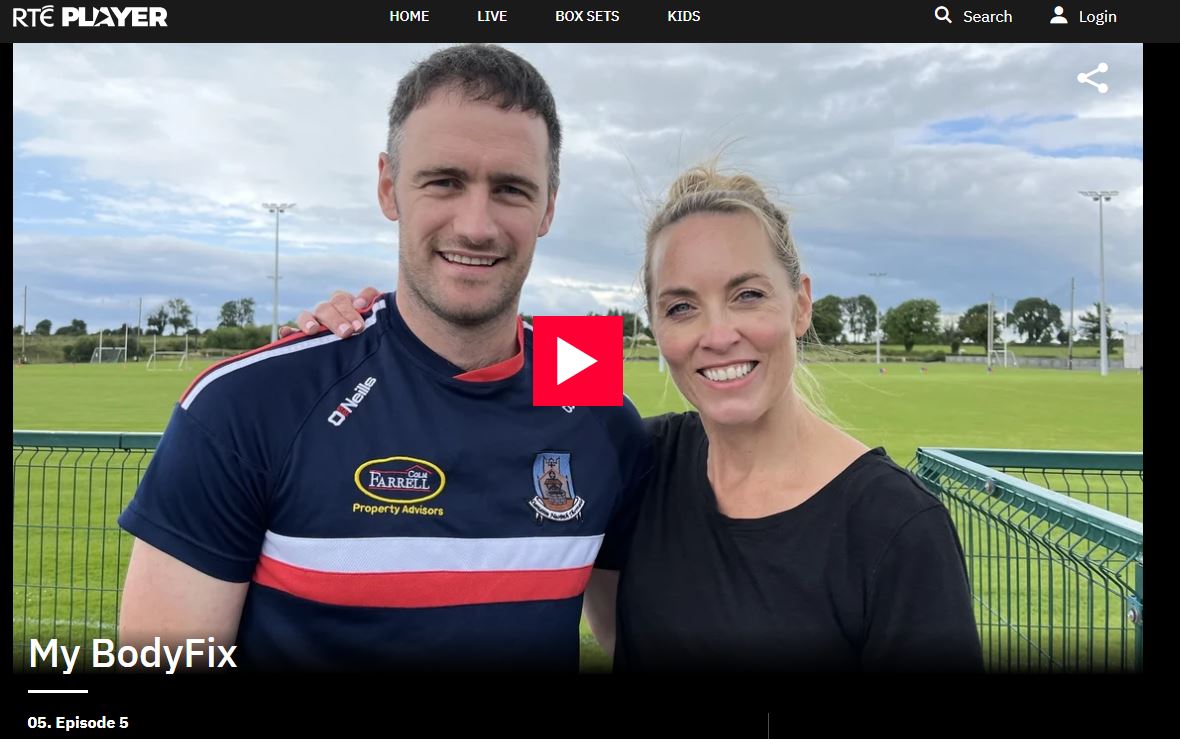
We’ve become great friends since and recently caught up to speak about work, life, injury prevention, strength and conditioning and more.
Andy: Tell us a bit about yourself – what got you into physiotherapy?
Liam: I attended Cushinstown primary school in Kilmoon, Ashbourne Community School, and then studied physiotherapy at Ulster University, Jordanstown, and completed a Masters Degree in Sport and Exercise Medicine.
The common theme for me throughout those years was Gaelic football and a love for sport and that’s why I felt physiotherapy would be a great career for me. In terms of my friends’ group and social aspects, I think it’s something that’s been very good to me, both professionally and personally as well.
Andy: Can you explain how we met?
Liam: Before I worked in Santry, I was working in Our Lady of Lourdes in Drogheda and also with the Meath football team and one of my best patients that came through was your mother, who was a far better patient than you…
We got talking and she said that you were struggling with your knee injury. I spoke about you with Colm Nally and he felt you were in a rut. I didn’t know if I could help but told him I would meet you for a chat. We met up at the Blues and you seemed very apprehensive. I thought you were very down at the time and I’d often find that with players who were injured who hadn’t previously experienced a serious injury. I felt you had lost a sense of identity, a purpose, and I remember we had a chat about just trying to pull everything back and not make any plans about returning to football.
You were struggling running, struggling day-to-day and we made a plan. As much as we’ve slagged each other, we’ve become good friends over the last few years and your attitude was brilliant.
Andy: Can you explain the injury I had?
Liam: I know you came with the MRI that you had and I think you may have had an injection. The way I describe an MRI – it’s fantastic to have such detailed imaging but we sometimes hang our hat on what the MRI shows.
An MRI is a still shot that doesn’t show how an athlete is moving, their strengths, their deficits, their weaknesses. We often find MRIs that may show damage on a scan but the patient can be pain-free and vice versa, patients can be in a lot of pain even though their scan looks fine.
We’d look at the clinical picture and looking back, you had a lot of physical deficits from right to left knee. We looked at your hip control, your lower limb strength, reactive strength and just your overall conditioning. We just had time together and again having worked with Meath,
I know what it’s like working in an inter-county set-up. You might only get a couple of minutes here and there with people so that’s why I really enjoy UPMC Sports Surgery Clinic.
You tend to get substantial time with athletes and can make a very individualised plan and sometimes it’s just time that players and athletes need and want. They want numbers and objective markers and a clear plan is of paramount importance.
Andy: You are working in the Sports Surgery Clinic in Santry. What do you do there?
Liam: When I finished as physiotherapist with Meath, thankfully, I obtained a PhD role through the University of Roehampton working as a physiotherapist in UPMC Sports Surgery Clinic. It is a brilliant environment to work in and is a world-renowned sports medicine centre.
I have some fantastic mentors in Colm Fuller, previous Irish rugby physio, he’s our lead physiotherapist. Dr Neil Welch is our head of research and lab services and adopted Newtown Blues man Thilina Vitharana, he’s one of the best physiotherapists I’ve ever met and just a genuinely great guy. He’s probably not the first transfer for the Newtown Blues and probably won’t be the last.
The sports surgery clinic would operate on approximately 2000 ACLs per year and the majority of those would be tested in the Sports Medicine Clinic. You have the main hospital and then there is sports medicine and that’s where I’m based.
I am currently leading the hip and groin service and I’m aiming to develop a hamstring service based off the back of my PhD. My PhD is looking at hamstring muscle strength and return to play. It’s an interesting injury at the minute because it’s the number one injury in sport that’s increasing.
If we look at Premier League injuries from last season to this season, they’ve spiked by 96pc. There’s a lot of questions as to why that’s happening and why hamstring injuries are becoming more prevalent.
Is it the way the likes of (Mauricio) Pochettino and Ange Postecoglou play with the high press, the high numbers? I’m not saying I have all the answers but I am hoping my research can assess and potentially improve how we manage hamstring injuries.
Andy: You were Meath physio and played with Curraha, how did you manage the workload?
Liam: As manic as those few years were, I really did enjoy them and learned so much. A lot of physiotherapists sacrifice their own playing careers to work with a team but I had very accommodating managers who allowed me to do both. I think both set-ups complemented each other.
Being a player with Curraha, I would have often ended up playing with and against some of the players I was treating. I learned a lot from Meath then and tried to bring back as much as I could to our own club in terms of standards, strength and conditioning, tactics and a culture overall.
To be fair, only for Bernie Hogan’s ready-made meals, I would have struggled to balance it all but my family were so helpful to me during that time and through my entire life supported me.
I grew up as a Meath and Curraha fan and to be able to combine both during two successful periods was something I will always cherish.
Andy: There is a lot of conversation currently around gym work and its role in the GAA. Is there too much strength work and not enough football? Could this be a cause of the ACL and hamstring injuries that we have seen occurring?
Liam: I recently had a conversation with a friend of mine, Tommy Mooney, our lead S&C coach in the SSC. You often hear the usual narrative ‘there were none of these hamstring injuries in my day’ but the fact of the matter is that the demands of modern football far exceed the game from years gone by. Players are stronger, faster and, in my opinion, this only adds to our game as a spectacle.
Strength and conditioning is a tool to enhance the physical qualities of our game and if it’s done well, should complement injury prevention. It should not supersede the game but should be done in conjunction with skill development.
| You need to have the baseline, physical characteristics as well as the ability to execute the skills of the game. The goal here is to find somewhere in the middle and that’s down to giving a personalised programme to each player based on what his needs are. |
Tommy had research published that looked at elite vs sub-elite U20 footballers and not surprisingly, the inter-county footballers were better in relation to body composition, speed, fitness and strength.
But when they examined the elite players only, there was no difference in those who started and those who didn’t. Basically, when these players reached a certain level of fitness, it came down to skill level.
Andy: What advice would you give to any GAA player for injury prevention?
Liam: It comes down to brilliant basics. A good, evidenced-based warm-up is of paramount importance for injury prevention. Preparing your body for what it will have to do in a game. Fifteen minutes of prep work before you get into a warm-up, looking at hip mobility, glute activation, eccentric hamstring work and some plyometrics.
I think if you cover these areas, you are on to a good thing. I had a small role in the ‘Activate’ warm-up run by Ulster GAA and the Sports Institute of Northern Ireland 10 years ago. If performed correctly, it can reduce non-contact ACL and hamstring injuries by 50pc.
Then, having a good S&C programme, whereby you have at least one weekly consistent lift that you can monitor and quantify by the weight you are lifting. Everyone wants a quick fix and to find this magic solution that no one else is doing. Mark Brady is Dublin’s lead S&C coach and you always hear people chatting and asking him the question, “What are you lads doing in there? Tell us your secrets?”
But they are doing the simple tasks to an extraordinary high level and they appear to have really good structures in place to facilitate this.
Andy: You work with the best of the best athletes, what sets them apart from the rest?
Liam: I suppose I’ve worked in a couple of sports, Gaelic football, athletics, AFL and rugby. A lot of these top elite athletes have a lot of the same characteristics. I think the openness and willingness to learn, looking for consistent feedback, and again it comes back to the brilliant basics.
What’s their attitude like? Again, you’ll know very quickly when you meet an athlete if he’s listening to what you’re saying but I think it works both ways. Any athlete I’ve met, I try to learn from them too and you can always learn from somebody else, and they’ll teach me about myself and I’ll often seek feedback on my end as well.
At the end of sessions I’ll ask, ‘why are they here?’ Really, what do they want to get out of it because if our train of thought is totally separate, we’re not going to go in the right direction.
If I’m seeing an ACL athlete, we need to build a level of trust and support. It means that I can call him out if I feel he’s not rehabilitating to a sufficient level and vice versa, if he feels that I’m not giving him the support that he needs. What sets those guys apart are the one percenters.
How can they communicate to the best of their ability, how can they improve their strength to the best of their ability, how can they seek feedback and if you’re consistently seeking feedback but also working on those pointers, I think you’re only going in the right direction. These athletes are extremely punctual, have great attention to detail and a real drive for continuous self-improvement.
Andy: You spent some time in Australia recently in different sporting settings. Can you explain what you do regarding Irish AFL players?
Liam: Initially, it started with Cian McBride, who was playing with Essendon at the time. He came home during Covid to play for Meath. We had an Irish guy, Conor Daly from Leitrim, who was head S&C coach with Essendon and we liaised closely with Cian’s rehab. Leading on from that, I had the opportunity to go and visit Carlton, Sydney Swans, Greater Western Sydney and St Kilda.
It’s phenomenal and makes you very proud as an Irish guy to see the level that some of our male and female athletes are reaching over there. I had a conversation with Patrick Cripps, who was the 2022 Brownlow Winner, and he spoke about the high level our Irish athletes are at. He described his own old housemate, (Ciarán) ‘Casey’ Byrne as a “gun” who had all the capabilities of being one of the club’s best players.
I have huge admiration for ‘Casey’ and I was travelling in 2017 with Robbie Brodigan, the Oliver Plunkett’s midfielder. We met him in Melbourne after he trained, 30 degrees, out sipping on a coffee, work done for the day and all I could think was how envious I was that this guy has it all.
But he was secretly homesick and he returned, won an intermediate championship, a senior league, fought back from an ACL injury and is back playing for Louth.
I would encourage anyone who wants to go to go but always say you’ll only realise how special your own club and home is when you are away.
I would screen a lot of the Irish guys who would go over in terms of their medicals and when they’re home, I would work on some of their rehabilitation with some players.
It’s interesting for my own development and learning because you’re putting your own thoughts and ideas on rehabilitation out to someone in a professional sports environment in Australia.
I was very lucky to do online consultancy work with a few of the clubs as well and it’s very enjoyable on a Saturday morning, switching on the TV and seeing maybe a guy or two that you worked with. We have some phenomenal athletes who are over there at the minute flying in the flag.
If these guys go over and they don’t make their debut, the learning they get, the maturity they have, they’re working in a professional environment and that’s something, unfortunately, that Gaelic games can’t give at the minute. I wouldn’t ever put a guy off going over and I think it’s an unbelievable opportunity.
Andy: Do you think your trip to Australia benefitted you in your work field/life?
Liam: We have so many similarities in terms of training methods but what they do in the AFL, they obviously have time to recover but they just do all the same things at a high level. In terms of our communication from physio to S&C to management, those structures work really well and there’s always clear pathways for players to get back.
I suppose I’m trying to bring that into any time I meet a player. The question everyone wants to know is when they’re back. But instead of saying this ACL injury is going to take 9-12 months before getting back, I break it down that to be running, we need your lower limb strength and reactive strength to be within 20pc to earn the right to run and within 10pc before looking at a return to play.
If you can map out to a player what those markers should look like prior to playing and work backwards from there and where they should be hitting, it’s a much easier conversation in three or six months if they’re not back running, that you have had the initial discussion that these were the non-negotiable scores that have not yet been achieved.
We often find that with a lot of our ACL injuries, they’re coming into clinic and, yes, they’re running but their running mechanics may not be sufficient because they have too much of a strength gap.
It’s easy for me to say, of course, we have great access to these testing devices in the SSC but I think we can be, as a profession, more objective-based as opposed to time-based.
You should always have an open mind and it’s about trying to learn from everybody – athletes, coaches and physiotherapists into what we can bring back into our own game.
They do a lot of craft, which is basically 15-20 minutes of skill work, in AFL. They work on ball drills and a lot of work on the ground ball, which is a bit more of a common theme in the AFL.
Though, leading on from that, as a physiotherapist, nothing equates to playing and I think that’s something I can’t get across enough. We’re only facilitating you guys as players.
The best day of my life was winning an intermediate championship with Curraha and I don’t think anything will ever get close to that.
I was lucky to have met Liam when I did, and I can’t thank him enough for instilling faith in me when it would have been easy to write off my injury. I don’t want to give him too much credit but I probably wouldn’t be playing football today if he hadn’t put in the effort and time with me that he did. Liam is an extremely charismatic guy and has been very successful to date in his career.
It’s not every day you hear me giving a Meath man praise…
| For further information or to make an appointment with one of the Sports Medicine Team at UPMC Sports Surgery Clinic, please email sportsmedicinessc@upmc.ie |