Osteoarthritis
Inflammatory arthritis
Treatment Advances in Inflammatory Arthritis
| For further information or to make an appointment with a Consultant Rheumatologist, please contact +353 1 526 2371 or email: rheumatologyssc@upmc.ie |
KNEE OSTEOARTHRITIS
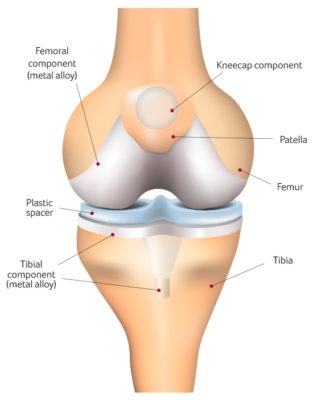
KNEE REPLACEMENT
Many patients have benefitted greatly from knee replacement, including many thousands of patients at SSC.
During a knee replacement, the orthopaedic surgeon removes severely degenerated cartilage and bone from the joint and substitutes it with artificial structures made from metal and plastic.
TREATING KNEE OSTEOARTHRITIS
| For further information on OPAS or to make an appointment please call 015262300 or email opas@sportssurgeryclinic.com |
WHAT CAN I EXPECT WHEN I ATTEND OPAS?
There are two main components to OPAS: an educational module and an individualized assessment
component.
Education Module (approximate duration 1.5 hours)
Each OPAS session commences with the Education component, where a small group of patients with OA will sit together and learn about OA. Our OPAS team have created a friendly and open environment that facilitates interaction and encourages discussion to enable you to learn as much as possible about your arthritis.
You will hear short talks from:
- The OPAS Rheumatologist (Dr Barry Sheane) explaining how OA develops, how it can be treated and how we can try and delay or even prevent joint replacement.
- The OPAS Physiotherapist advising about the importance of exercise in treating OA and how we can help you begin an exercise regimen designed with your specific needs in mind.
- The OPAS Dietician on how your diet can be used as a way to reduce pain/manage OA through healthy eating and/or losing weight.
These talks will be informal and we strongly encourage patient-speaker interaction during the Education module!
Understanding OA is a key component in any treatment strategy and the OPAS team welcome any and all questions.
Assessment Module (approximate duration: 1.5 hours)
The Assessment Module is the second part of OPAS. You will be individually assessed by the Physiotherapist
and Dietician.
- The Physiotherapist will assess the range of motion in your affected joint(s), identify any muscle weakness that might be contributing to your OA, and check the alignment of the joints in your legs. Based on this information, you will receive an individualized treatment and exercise plan to help maximize your mobility and enhance your participation in the daily activities that you enjoy most.
- The Dietician will assess your weight, body mass index (BMI) and daily diet. Based on this information, you will receive advice on how to eat healthily in OA, and how you can change your daily diet to help lose weight, thus unloading excess pressure from the joints in your legs and reducing pain.
| For further information on OPAS or to make an appointment please call 015262300 or email opas@sportssurgeryclinic.com |
HOW LONG IN TOTAL WILL I BE AT THE HOSPITAL FOR OPAS?
You will be at the Hospital for approximately 3 hours on the day of your attendance at OPAS. However, as OPAS is delivering individualised treatment for each patient, these times may be longer (or shorter).
IS THERE ANYTHING I NEED TO DO BEFORE I ATTEND OPAS?
Before attending OPAS, you will receive a number of questionnaires relating to your OA. Kindly complete these questionnaires and bring them with you on the first day of OPAS.
These completed questionnaires will help the OPAS team understand your pain level, how OA is affecting your day-to-day activities and your mood, and will assist us in devising a treatment programme that works best for you.
You will also be asked to complete a ‘food diary’ for 5 days prior to attending to help us advise on your diet.
WHAT HAPPENS IMMEDIATELY AFTER MY OPAS ASSESSMENTS?
Following these two assessments, you will conclude your visit with the OPAS Nurse.
The Nurse will review with you the advice and instructions you will have received from the Physiotherapist and Dietician and answer any questions you might have about your treatment plan.
WHAT HAPPENS IN THE WEEKS AFTER ATTENDING OPAS?
You will have access to two additional interactive group sessions taken by the OPAS Dietician.
Each of these sessions will cover a different topic relating to diet/ weight loss and arthritis, including Eating Habits and Barriers to Weight Loss.
There will be time at the end of each of these sessions to discuss your individual progress with the Dietician.
Two additional sessions with the OPAS Physiotherapist will also be available if you so require as part of the comprehensive package from OPAS.
As additional support, after the Dietician’s talks, the OPAS Nurse will also be available to discuss your progress and address any ongoing difficulties you may be experiencing with your individualized OPAS exercise and dietary plan.
The Nurse will assist you as necessary in helping you progress with your treatment.
DO I NEED TO BE REFERRED BY A DOCTOR TO OPAS?
In order for the OPAS team to deliver individualized treatment specifically for Osteoarthritis, patients require a formal consultation from an Orthopaedic Surgeon, Sports Physician or Rheumatologist prior to attending OPAS, in order to confirm patient suitability.
HOW MUCH DOES IT COST TO ATTEND OPAS?
The cost of attending OPAS is €300. This will cover three interactive sessions with the OPAS Dietician, a comprehensive assessment from the OPAS Physiotherapy Team, design and prescription of an individualized physio and exercise programme tailored for your specific needs, two follow-up sessions with the OPAS Physio Team to address any difficulties requiring additional input, and follow-up and support from the OPAS Nurse Co-ordinator.
In addition, this cost will include access to the Educational component of OPAS, including an educational lecture about OA from Dr Barry Sheane (Consultant Rheumatologist) and on ‘Exercise and OA’ from the OPAS Physiotherapy Team.
| For further information on OPAS or to make an appointment please call 015262300 or email opas@sportssurgeryclinic.com |